Developing New Vascular Access Technologies to Improve Outcomes
Founded in California’s Silicon Valley, Solinas Medical’s mission is to address the greater than $3 billion costs associated with cannulation-related complications in patients undergoing hemodialysis. We are partnered with leading physicians to improve patients’ lives through innovation.
Vascular Access Issues Are Costly and Result in Poor Outcomes
- ESRD patients comprise approximately 1% of Medicare beneficiaries but account for nearly 7% ($33 billion) in total costs [1].
- The 5-year cumulative cost of maintaining AV graft access exceeds $15,000 per patient [2].
- Central line-associated bloodstream infections (CLABSIs) are a leading cause of hospitalizations and the second leading cause of death in hemodialysis patients with a mortality rate of 12%-15% and an estimated total direct and indirect costs associated with hospitalizations ranging from $17,000 to $32,000 per episode [3-6].
- The ESRD Quality Incentive Program has not achieved CMS’ stated goal of reducing long-term TDC utilization rates below 10% [7].

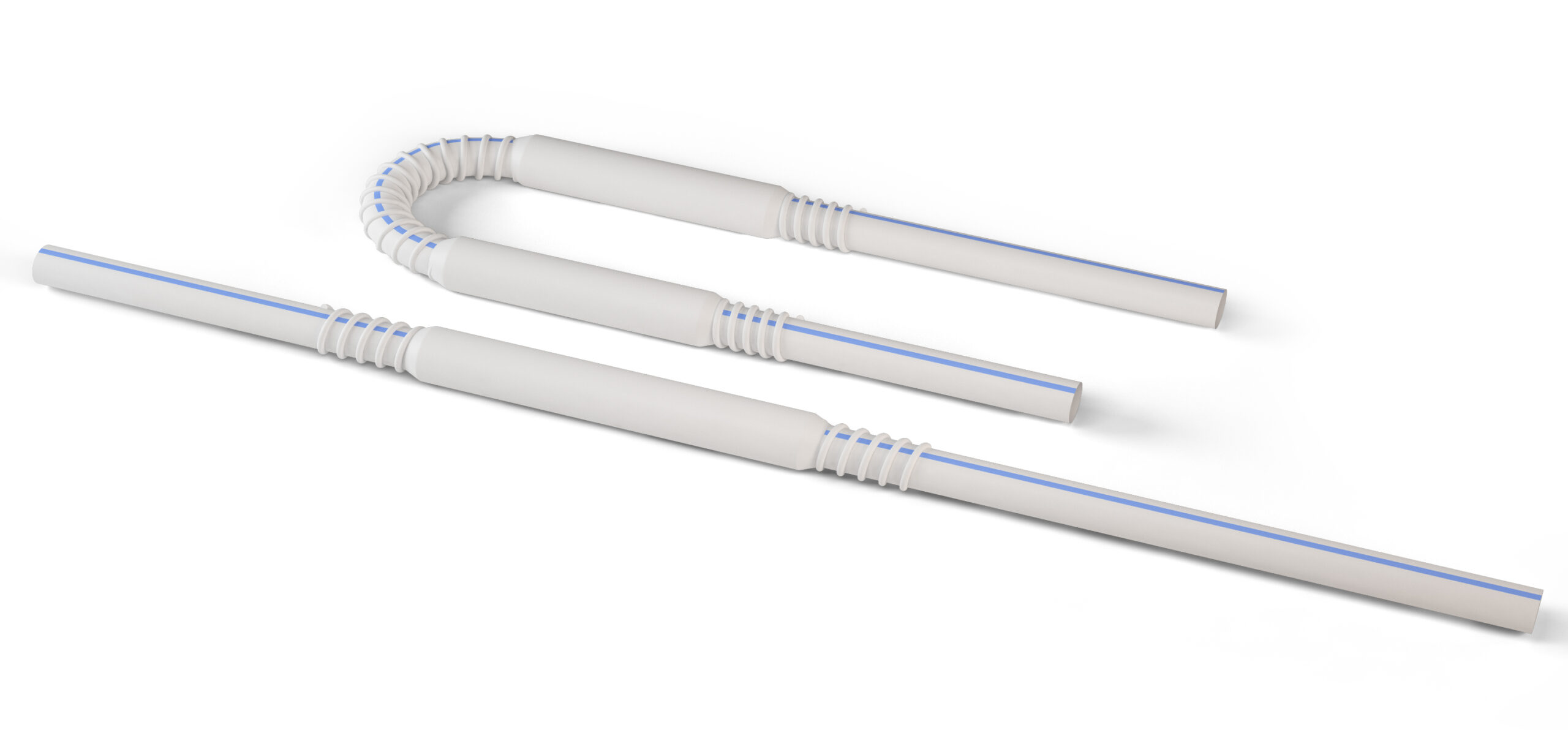
The ReTAP AV Graft® Aims to Improve Outcomes
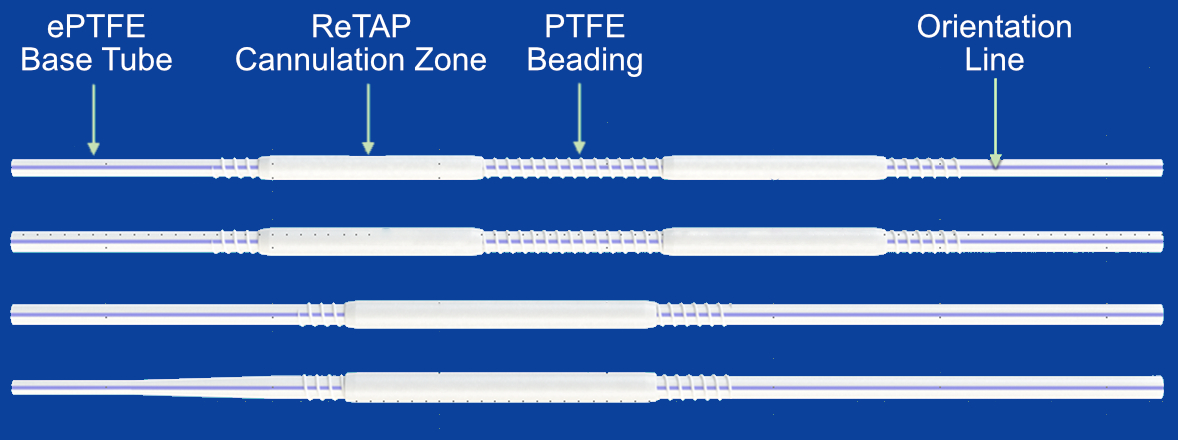
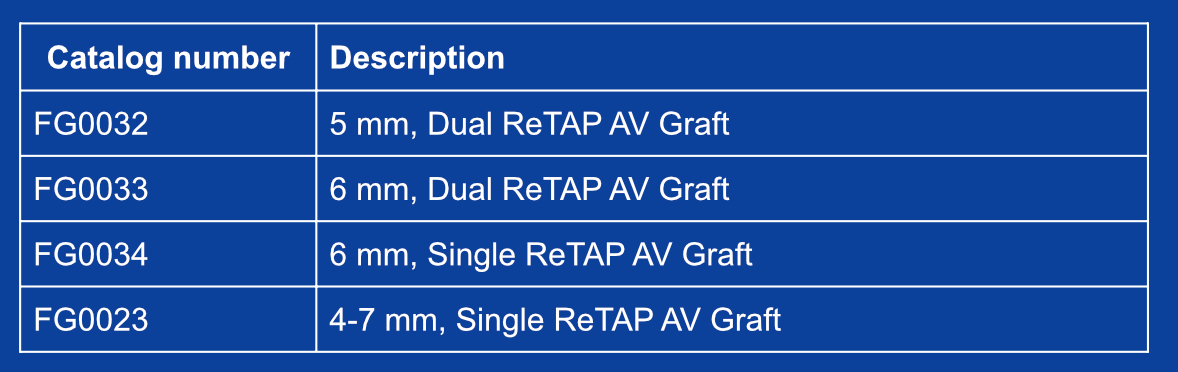
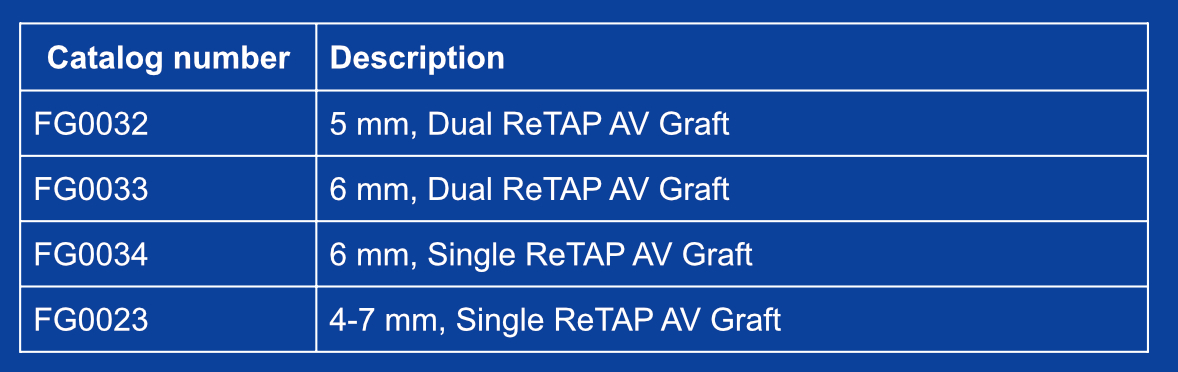
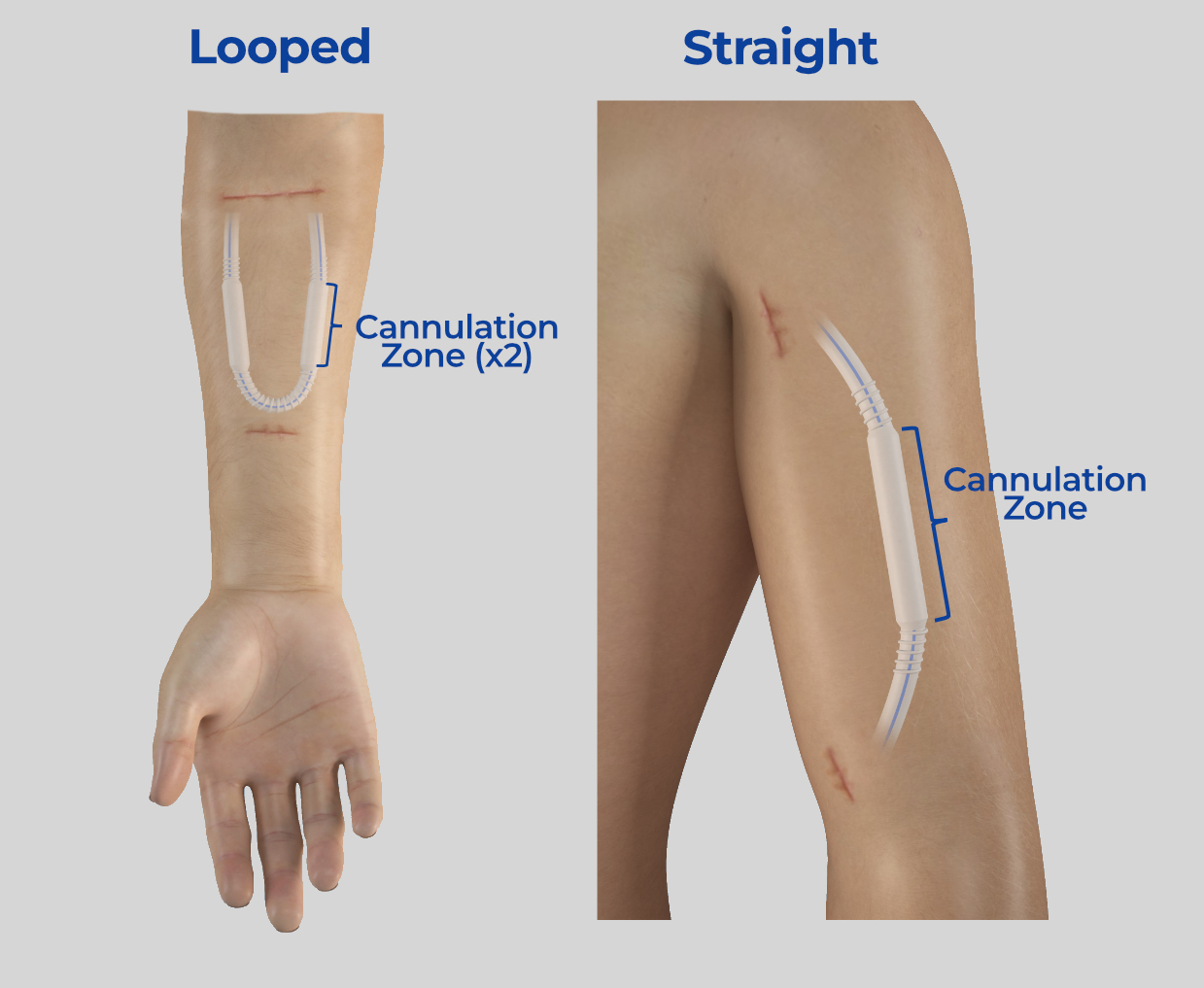
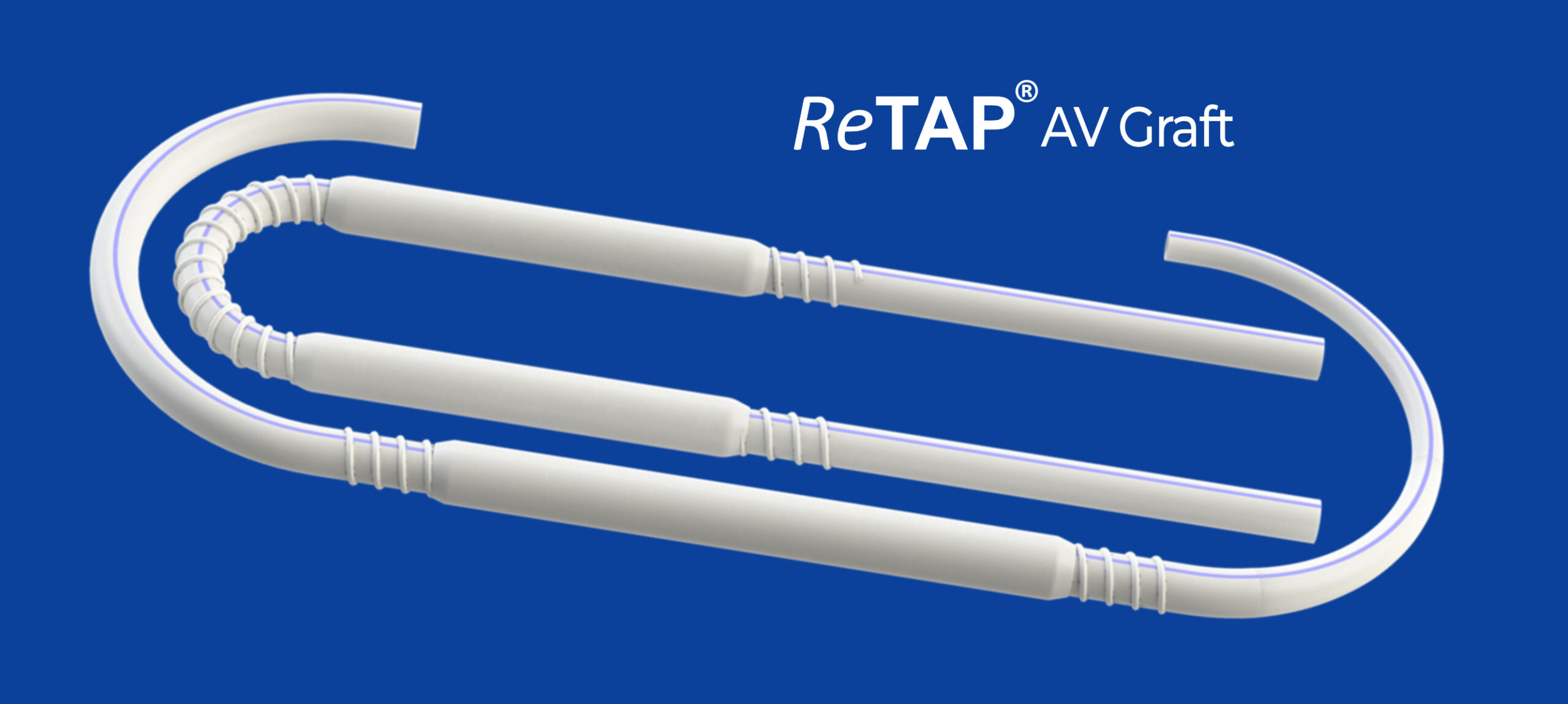
The ReTAP AV Graft has one or two ReTAP zones with enhanced sealing performance. The ReTAP zones are fully integrated with the base ePTFE tubing to avoid pockets or chambers in which blood or other bodily fluids could collect.
- Leverages traditional ePTFE tubing platform to optimize hemocompatibility and suture-ability.
- ReTAP zones enhance leak resistance to support early AVG cannulation, which has the potential savings of $3,169 per patient and reducing tunneled dialysis catheter use by 18.5 days [6].
- ReTAP AVG maintains the same surgical methods as traditional AV grafts for device placement.
- ReTAP AVG maintains the same cannulation methods for device hemodialysis treatment, including enhanced palpation and permitting cannulation anywhere around its circumference.
1. United States Renal Data System. 2023 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2023.
2. Sorber R, Canner JK, Abularrage CJ, et al. Quantifying The Costs of Creating and Maintaining Hemodialysis Access in An All-Payer Rate-Controlled Health System. Ann Vasc Surg. 2021;76:142-151. doi:10.1016/j.avsg.2021.05.008
3. Nguyen OB, Shugart A, Lines C, et al. National healthcare safety network (NHSN) dialysis event surveillance report for 2014. Clin J Am Soc Nephrol 12(7), 1139-1146, 2017.
4. United States Renal Data System. 2018 USRDS Annual Data Report: Epidemiology of kidney disease in the Unites States. National Institutes of Health, Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2018.
5. Ziegler MJ, Pellegrini DC, Safdar N. Attributable mortality of central line associated bloodstream infection: systematic review and meta-analysis. Infection. 2015;43(1):29-36. doi:10.1007/s15010-014-0689-y
6. Kosa SD, Lok CE. The economics of hemodialysis catheter-related infection prophylaxis. Semin Dial. 2013;26(4):482-493. doi:10.1111/sdi.12115
7. Shah S, Feustel PJ, Manning CE, Salman L. CMS ESRD quality incentive program has not improved patient dialysis vascular access. J Vasc Access. 2023;24(2):246-252. doi:10.1177/11297298211027054